Lymphoid organs are specialised tissues where lymphocytes develop, mature and differentiate. They are divided into primary lymphoid organs, where lymphocytes develop, and secondary lymphoid organs, where adaptive immune responses are initiated (Figure 1.2).
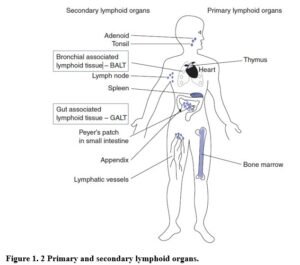
Primary lymphoid organs – bone marrow and thymus. В and T cells originate in the bone marrow but only В cells mature here (bone marrow derived). T cells migrate to the thymus for maturation (thymus derived). Once maturation is complete, both types of cells enter the bloodstream and migrate to the peripheral lymphoid organs.
Secondary lymphoid organs. Secondary lymphoid organs are organised to trap antigen from sites of infection, facilitate antigen presentation to lymphocytes and provide the optimal microenvironment for lymphocyte maturation. They include lymph nodes, spleen and mucosa-associated lymphoid tissue (MAI.T) and all share the same basic structure. Immune responses are initiated in secondary lymphoid tissues.
Lymph nodes. Lymph nodes trap antigens from sites of infection in tissue (Figure 1. 3). Afferent lymphatic vessels transport extracellular tissue fluid (lymph) carrying antigen and APCs to the lymph nodes. In lymph nodes, В cells are concentrated in follicles and T cells are distributed in the surrounding paracortical area (T cell zone). When В cells encounter their specific antigen and antigen-specific helper T cells, they proliferate in germinal centres of the follicles. The organisation of lymph nodes and other secondary lymphoid tissues promotes В cell interaction with helper T cells, which is essential for antibody responses.

Spleen. The spleen collects antigens from the blood. The main bulk of the spleen is red pulp, the site of red blood cell (RBC) disposal. Lymphocytes surround arterioles entering the spleen forming areas of white pulp, which are divided into the peri-arteriolar lymphoid sheath (PALS), containing mostly T cells, and the В cell corona. Lymphocytes and antigen-loaded dendritic cells come together in the PALS.
Mucosal-associated lymphoid tissue. MALT includes the gut-associated lymphoid tissue (GALT), bronchial-associated lymphoid tissue (BALT) and aggregates of lymphocytes in other mucosae. GALT collects antigen from the epithelial surfaces of the gastrointestinal tract (GIT) and includes the tonsils, adenoids, appendix and specialised structures called Peyers patches in the small intestine.
The mucosal surfaces are particularly vulnerable to infection. The immune system must avoid responding to food antigens, while still detecting and killing pathogens. The MALT lining the gut is known as gut-associated lymphoid tissue or GALT and includes tonsils, adenoids and Peyer’s patches.
PEYER’S PATCHES Peyer’s patches facilitate induction of immune responses in the small intestine. Specialised epithelial cells called M cells form a membrane overlying the lymphoid tissue and take up antigens from the gut lumen by endocytosis. Antigens are transported through M cells and delivered directly to APCs (dendritic cells) and lymphocytes of the mucosal immune system.
A DISTINCTIVE REPERTOIRE OF LYMPHOCYTES There are small foci of lymphocytes and plasma cells scattered widely throughout the lamina propria of the gut wall. These are effector cells of the gut mucosal immune system and the T cells can be divided into conventional αβ-T cells and γδ-T cells. Naive lymphocytes leave the thymus and enter the mucosal immune system via the bloodstream. On encountering foreign antigens, lymphocytes are activated and traffic, via the lymphatics through mesenteric lymph nodes, to the thoracic duct and circulate in blood throughout the entire body. They re- enter mucosal tissues including other sites of MALT (respiratory and reproductive mucosa). Hence immune responses initiated in Peyer’s patches are disseminated throughout mucosal sites. This pathway of lymphocyte trafficking is distinct from and parallel to that of lymphocytes in the rest of the lymphoid
system.
SECRETORY IgA The major antibody isotype present in the lumen of the gut is secretory polymeric IgA, synthesised by lamina propria plasma cells and transported into the gut lumen. Polymeric IgA binds mucus overlying the gut epithelium, acting as an antigen-specific barrier to pathogens and toxins.
MOST ANTIGENS PRESENTED TO THE MUCOSAL IMMUNE SYSTEM INDUCE
TOLERANCE The mucosal lymphoid system is exposed to many foreign antigens from foods and commensal bacteria to pathogenic microbes and parasites. Immune responses to food antigens are rarely detected. Feeding foreign antigens leads to specific, active unresponsiveness – known as oral tolerance. In contrast, pathogenic microorganisms induce strong TH1 responses.
The context in which peptide is presented to T cells of the mucosal immune system appears to determine whether tolerance or a powerful adaptive immune response ensues. In the absence of inflammation, presentation of peptides to T cells by MHC molecules on APCs occurs without adequate co-stimulation. However, pathogenic organisms induce inflammatory responses, which stimulate maturation and expression of co-stimulatory molecules on APCs. Subsequent antigen presentation favours development of a TH1 response.
Lymphocyte trafficking Lymphocytes express adhesion molecules, with which they attach to endothelial cells prior to migrating into tissues or lymphoid organs. Some lymphocytes have specific adhesion molecules (addressins), which bind to ligands on endothelial cells in particular vascular beds, for example, mucosal lymphocytes express addressins which favour migration into MALT.
Naïve T and В cells are mature lymphocytes that have not yet encountered antigen. These cells continually migrate into the secondary lymphoid tissues via the bloodstream. They return to the blood via the (efferent) lymphatic vessels and the thoracic duct. Naïve lymphocytes recirculate until they meet their cognate antigen. If this docs not occur they die.
When pathogens enter the body, APCs (c.g. dendritic cells) take up and process antigen. APCs and free antigen are carried in afferent lymphatics to regional lymph nodes. Here APCs display processed antigen to recirculating T lymphocytes, activating antigen-specific cells. Activated T cells proliferate and differentiate into antigen-specific effector cells and leave the lymph node via efferent lymphatics, re-enter the blood stream and migrate to the site of infection.
Recirculating В cells that encounter antigen are activated, proliferate and differentiate into antibody- secreting plasma cells. Plasma cells may remain in the lymph node or return to the bone marrow (via efferent lymphatics and bloodstream).
All secondary lymphoid tissues trap APCs and antigen, present it to migratory lymphocytes thus stimulating an adaptive immune response. В cell follicles of the lymph nodes expand and proliferate to form germinal centres and the entire lymph node enlarges – giving rise to swollen glands.